Over the past few years the field of Shared Decision Making has developed rapidly. The main topic of discussion these days is: How can we move to structural implementation? Marjan Faber of IQ healthcare, Radboudumc, organised a workshop today together with Glyn Elwyn from the PreferenceLab, Dartmouth College. Here you can read a short summary of the workshop.
Researchers behind the MAGIC and CollaboRATE programmes were invited to share their experiences. Also current initiatives within the Netherlands were presented by NPCF, Maastricht UMC+ and Radboudumc.
Measuring effects to fuel implementation
Amy Lloyd from Cardiff University and Rachel Thompson from Dartmouth College shared their experiences on SDM measurement tools.
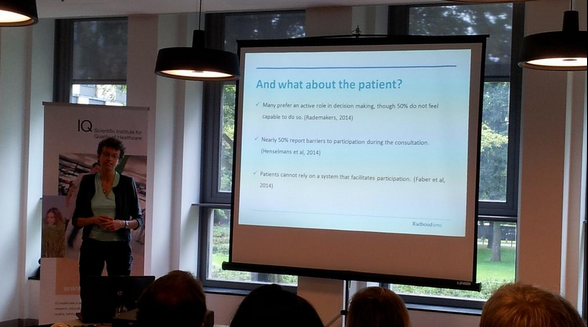
What to measure is not evident. Patient satisfaction is too broad, since this is more linked to service oriented aspects, such as waiting time. Regret has often been used as a measure, but what does it entail exactly and how does timing of measurement influence the outcome? Another option is the quality of the decision, which measures how well the patient preference matches with the chosen treatment. Patient involvement in the decision process is arguably a good measure, but also complex.
Amy shared insight on the five tools she tested in the MAGIC programme: team feedback tool, SDM questionnaire, OPTION instrument, Decision Quality Measure and the SURE test. Her main conclusions were:
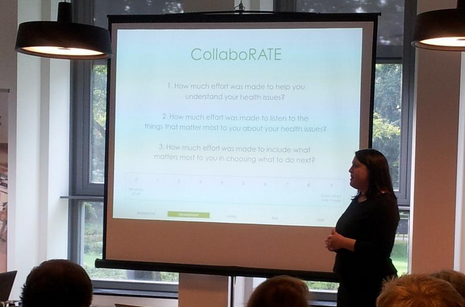
Rachel explained that a main goal of CollaboRATE is to develop generic, valid and scalable way of measuring SDM.
In co-creation with patients three questions were developed to measure the perceived SDM by the patient:
The patients give a score from 0 (No effort at all) to 9 (Every effort was made). The aim being the gold standard, a positive score was only given when the patient scored a 9 on all three questions.
This method was tested with over 5000 patients in 19 centers. Main conclusions are: that the questionnaire is understandable, useful and can be done in 30 seconds. There was a huge variation in scores between teams, from patients evaluating 4% as the gold standard to 96%. The teams use their score to improve their daily practice and top teams are helping lower scoring teams by sharing their insights.
Trudy van der Weijden from Maastricht UMC+ introduced her project to develop an SDM intervention for breast cancer, to reduce practice variation. She plans to measure the effect by the OPTION 12 questionnaire, because there are a lot of references available for benchmarking. She is considering using the OPTION 5 questionnaire because it’s more compact.
To record or not to record?
With the rise of the smartphone, it has become very easy to make a digital recording. Glyn Elwyn introduced an interesting discussion on the trend of patients recording their consultation, with or without consent of their doctor. The main reason being: "I want to remember what is told to me". There are a few questions to consider:
In some fields, such as pediatrics, it’s common practice for the healthcare provider to offer a recording to the patient for the past 30 years. This has been highly valued by patients as a useful tool to recall the consultation for better understanding. Yet in other areas this is not common practice at all.
Recording the consultation for recall by patients would transform the black box into a transparant consultation that can easily shared with loved ones. We need to find the right conditions so both doctors and patients feel comfortable with this. Join the discussion at BMJ here.
Empowering the patient
Following the successful "Ask 3 Questions" campaign in Australia and the UK, Anouk Knops of NPCF presented their plans for initiating a Dutch campaign. Most interesting conclusions were that the three questions: give patients permission to be involved in the decision making; the quality of information given was higher; and there was no difference in length of consultation.
Additionally research done among NPCF members show that 98% want to be involved in the decision making but 63% did not receive a choice between multiple options. The team is now finalizing the Dutch campaign, which will start with a pilot at Radboudumc before a nationwide implementation.
Marjan Faber presented the idea of the Patient Academy and asked the audience for feedback. This goal of the academy is to empower patients by teaching and training them. Courses would include:
During the discussion that followed the patients need was validated. It is important to think about how patients are approached and who is teaching the courses. It was suggested that patient representatives should play an important role.